Infection Prevention & Control Guidelines within Home Care & Community Care Settings
The current outbreak of coronavirus disease (COVID-19) is caused by a newly identified virus, the SARS coronavirus2 (SARS-CoV-2). Most people with COVID-19 have only mild symptoms and do not require admission to hospital. However, some have developed severe illness and deaths have been reported. There is evidence that COVID-19 can be spread from people who are sick to others with whom they have close contact. Close contact involves situations such as caring for, or living with someone who is ill.
Organizations, agencies, and individuals that provide health care to clients in their home/community setting need to be prepared to look after individuals with COVID-19 (suspected and confirmed). The guidance in this document is intended for care providers who see clients in their home/community setting. It will be updated as new information becomes available.
Screening and Triage Home Care and Community Care services will conduct passive and active screening of clients and their families. Passive screening for clients and their families All clients should be asked to report fever > 38 degrees Celsius and/or new or worsening cough in themselves or a household member to the Home Care and Community Care services provider before the visit at a number provided to them. Active screening for clients and their families
All clients and their household members should be screened for COVID-19 by a designated staff member (e.g., continuing care assistant, nurse, scheduler, manager, and other health care professionals) by phone the day of the scheduled visit. The following screening questions should be asked of client and household members: Do you have?
1. Fever (temperature over 38 degrees Celsius) OR symptoms of a fever (no thermometer available) AND/OR new onset or worsening of chronic cough
AND any of the following:
2. Travel outside of Canada in the 14 days before the onset of illness OR close contact with a confirmed or probable case of COVID-19 OR close contact with a person with acute respiratory illness who has been outside of Canada in the 14 days before their symptom onset. NOTE: Screening questions are subject to change through direction of the office of the Chief Medical Officer of Health, DHW. Staff should also ask if other people will be in the home during the appointment (e.g. nonhousehold visitors) and ask them the screening questions as well. Clients, household members, and/or non-household visitors in the home who answer yes to screening questions 1 and 2 should be directed to contact 811 for advice on the most appropriate setting for clinical assessment and testing (if warranted).
If the client or household member states that they are very ill, the staff person should advise the client/household member to contact 911 (EHS) as they may require emergent care. If the client and/or household member is suspected to have or has tested positive for COVID-19 and is self-isolating or recuperating at home:
• Necessary client care will continue using the infection prevention and control guidance as below.
• All Non-Urgent care should be postponed. Examples: Can non-essential housekeeping be postponed until the client does not require additional precautions? Can physiotherapy or occupational therapy be postponed until the client does not require additional precautions? Can non-urgent care coordinator assessments or reassessments be postponed until the client does not require additional precautions? Conduct assessments (e.g. care coordination) via phone as much as possible.
Infection Prevention & Control Guidance for Caring for a Client with Suspected or Confirmed COVID-19
Care providers will, in addition to Routine Practices, implement Droplet & Contact Precautions and use the correct personal protective equipment when within 2 metres of the client. *In some circumstances the client may not be a suspected or confirmed case, but a member of the household/family member is. Any symptomatic people in the household should be asked to remain in another room during the visit. Droplet and Contact Precautions should still be initiated.
Routine Practices
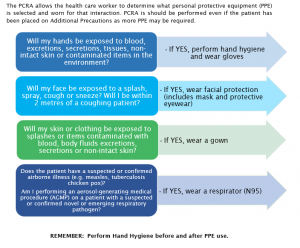
Routine Practices should be consistently used with all clients. The key to implementing Routine Practices is for care providers in home care/community settings is to conduct a Point of Care Risk Assessment (PCRA) with each client interaction. The PCRA will assess risk of transmission of microorganisms and assist staff to choose interventions or infection control measures to use. This includes assisting the health care worker to select the appropriate personal protective equipment (See Appendix A).
Droplet & Contact Precautions
For cases of suspected or confirmed COVID-19, Additional Precautions (Droplet and Contact) will be implemented. Droplet and Contact Precautions include:
• Ensuring that for any visit, the health care worker has the appropriate supplies, including personal protective equipment (PPE), to make certain that the additional precautions are maintained.
• Ensuring the home/community setting has a safe place to put on and remove PPE.
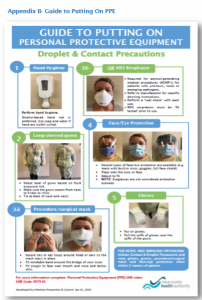
• Performing Hand Hygiene, with an alcohol-based hand rub or soap and water, whenever indicated (Four Moments of Hand Hygiene), paying particular attention to during and after removal of PPE, and after leaving the client care space.
• Dedicating client care equipment or ensuring all equipment (e.g. stethoscope) is cleaned and disinfected between clients with a hospital-grade disinfectant/wipe. If paper forms must be completed and signed by the client: use a disposable pen that can be left in the home and use a plastic clipboard that can be wiped down with disinfectant. The papers can be placed in a folder and usual processes followed.
• Cleaning of the client care environment using a disinfectant wipe as necessary. Attention should be paid to high touch surfaces.
• Using appropriate personal protective equipment (PPE) for Droplet and Contact precautions. This includes gloves, long-sleeved gown, procedure/surgical mask and eye/face protection.
• Avoiding doing aerosol-generating medical procedures (AGMPs) in the home. Alternative therapy should be explored when possible including use of alternatives such as meterdosed inhaler with spacer instead of nebulizer. If an AGMP (e.g. nebulized therapy) is necessary and unable to be administered by the client or household member, it should be administered by nursing staff trained in the use of Additional Precautions. A fit tested respirator (N95) is required in addition to Droplet and Contact precautions. The respirator is not removed until after leaving the client’s home.
• Ensuring proper training in putting on and removing PPE in order to prevent crosscontamination and the potential spread of infection (refer to attached NSHA signage in Appendix B & C) and the following video.
After applying the required PPE, the care worker should instruct the client to wear a procedure mask (if tolerated) while the care worker is providing care. Clients should also be instructed on respiratory/cough etiquette including sneezing/coughing into their elbow or tissue, putting used tissues into a waste receptacle and performing hand hygiene immediately following.
The duration of Droplet and Contact Precautions should be determined in consultation with Public Health.
Household members, family members, private caregivers who are also involved in caregiving for the client can be directed to the following Public Health Agency of Canada webpage: Coronavirus disease(COVID-19): How to care for a person with COVID-19 at home- Advice for caregivers. It offers advice on preventative measures that can be utilized in the home environment.
Employee Health
• Care providers who become ill with a respiratory infection should report their illness to their organization and follow established protocols. • If COVID-19 is suspected or diagnosed in a care provider, case management and return to work should be determined in consultation with local public health/Medical Officer of Health. Ill care providers should not work at any healthcare facility or organization until cleared to return to work.
Specimen Collection and Testing
At this time, home and community care providers are not expected to conduct testing for COVID19. All health care providers have a duty to report a client who has or may have COVID-19 to their local Public Health Offices. The care provider should refer them to 811 for the most appropriate setting for the client to be clinically assessed and tested.
For more information:
NSHA Coronavirus Disease (COVID-1) webpage Nova Scotia Department of Health and Wellness Novel coronavirus (COVID-19) webpage
References: Nova Scotia Department of Health. Coronavirus Webpage. Ontario Ministry of Health. Novel Coronavirus (COVID-19) Guidance for Home and Community Care Providers. (February 11, 2020). Public Health Agency of Canada (2020). Infection Prevention and Control for COVID-19: Interim Guidance for Acute Healthcare Settings
Province of Nova Scotia. (2019). Respiratory Response Plan for Public Health (including SARI, novel influenza and novel coronaviruses) 2019-2020. Province of Nova Scotia. (2020). Nova Scotia Interim Guidance: Public Health Measures of cases and contacts associated with Novel Coronavirus (COVID-19). Date: March 4, 2020
Appendix A- Point of Care Risk Assessment (PCRA) Point of Care Risk Assessment
Before each patient/resident/client interaction, the health care worker completes a ‘Point of Care Risk Assessment’ (PCRA) by asking the following questions to determine the risk of exposure and appropriate Routine Practices and Additional Precautions required for safe care:
• What are the client’ symptoms?
• What is the degree of contact?
• What is the degree of contamination?
• What is the client’s level of understanding and cooperation?
• What is the degree of difficulty of the procedure being performed and the experience level of the care provider?
• What is my risk of exposure to blood, body fluids, excretions, secretions, non-intact skin and mucous membranes?
The PCRA allows the health care worker to determine what personal protective equipment (PPE) is selected and worn for that interaction. PCRA is should be performed even if the patient has been placed on Additional Precautions as more PPE may be required.